Men carrying mutations in the so-called “Jolie gene” – the BRCA 1 and BRCA 2 genes – face a significantly higher risk of developing aggressive prostate cancer, according to new research from the Institute of Cancer Research in London.
Understanding the BRCA Mutation
What are BRCA 1 and 2 Genes?
BRCA 1 (BReast CAncer gene 1) and BRCA 2 (BReast CAncer Gene 2) are genes that produce proteins that help repair damaged DNA. Everyone has two copies of each of these genes—one copy inherited from each parent.
People who inherit a harmful change (also called a mutation or pathogenic variant) in one of these genes have increased risks of several cancers—most notably breast and ovarian cancer, but also several other types of cancer. People who have inherited a harmful change in BRCA1 or BRCA2 also tend to develop cancer at younger ages than people who do not have such a variant.
Nearly everyone who inherits a harmful change in the BRCA1 or BRCA2 gene from one parent has a normal second copy of the gene inherited from the other parent. Having one normal copy of either gene is enough to protect cells from becoming cancer. But the normal copy can change or be lost during someone’s lifetime. Such a change is called a somatic alteration. A cell with a somatic alteration in the only normal copy of one of these genes doesn’t have sufficient DNA repair ability and can become cancer.
National Cancer Institute
The BRCA 1 and BRCA 2 genes normally act as DNA repair mechanisms, helping to protect against cancer by fixing damaged genetic material. However, around one in 400 people carry a faulty version of these genes. These mutations can dramatically increase the risk of certain cancers, including breast, ovarian and prostate cancer.
The genes became widely known as the “Angelina Jolie genes” after the actress revealed in 2013 that she carried a BRCA 1 mutation and chose to undergo a preventative double mastectomy to reduce her cancer risk.
What the Study Revealed
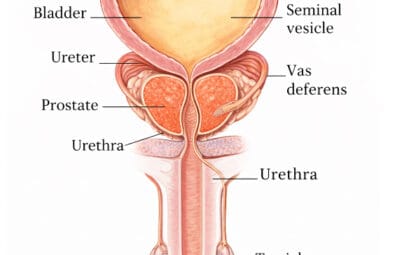
The new study, presented at the European Society for Medical Oncology (ESMO) congress, followed 3,064 men aged between 40 and 69 over a five-year period. More than half of the participants carried a BRCA 1 or BRCA 2 mutation. Each man received annual prostate-specific antigen (PSA) blood tests, which are used to detect possible signs of prostate cancer.
Researchers found that:
- Men with BRCA 2 mutations were more than twice as likely to develop prostate cancer.
- Men with BRCA 1 mutations were three times as likely to be diagnosed with an aggressive or clinically significant form of the disease.
- BRCA 2 carriers tended to develop prostate cancer at a younger age — on average at 60 years old, compared with 65 for those without mutations.
These findings underline the urgent need for targeted NHS screening among high-risk men.
Calls for Early and Targeted PSA Screening
Professor Rosalind Eeles, who led the research at the Institute of Cancer Research, emphasised that early detection is key:
“Our research shows that men with BRCA 1 and BRCA 2 mutations face a significantly higher risk of aggressive prostate cancer. Until more accurate diagnostic tests become available, targeted PSA screening in this high-risk group could detect these cancers earlier, when treatment is more effective.”
The research team has urged UK health authorities to update national guidance, recommending that all men aged 40 and over with BRCA mutations should be offered annual PSA testing.
The National Screening Committee is due to review whether a new targeted screening programme should be introduced. While the committee is expected to maintain that mass PSA testing carries more risks than benefits, it may endorse screening for high-risk groups, including men with a family history of prostate cancer and Black men, who are statistically more likely to develop the disease.
However, recent guidance has confirmed that national prostate cancer screening has been refused in the UK. Following a review of the available evidence, the UK National Screening Committee concluded that a mass screening programme using current tests would risk overdiagnosis and unnecessary treatment, with no clear overall benefit for the general population. While limited screening has been recommended for men with certain high-risk genetic markers, most men will not be routinely invited for testing. The decision and its implications are explained further by Prostate Cancer UK.

Late Detection of Prostrate Cancer and Claiming Compensation
If you feel this has occurred contact us now, we are here to help.
Contact Us Now To Claim
The Challenge with PSA Screening
Although PSA testing remains the standard tool for detecting prostate cancer, it is far from perfect. Elevated PSA levels can indicate cancer, but they may also result from benign conditions such as prostate enlargement or infection. Conversely, some aggressive cancers do not produce high PSA levels, leading to false negatives.
False positives can cause unnecessary anxiety and treatment, with potential side-effects such as incontinence and erectile dysfunction. Despite its limitations, researchers believe PSA testing is currently the best available tool for early detection in high-risk groups.
Pros and cons of prostate screening by Yorkshire Cancer Research:
Pros:
- This can help to pick up prostate cancer before you have any symptoms.
- Can help to pick up fast-growing cancer at an early stage, meaning treatment can stop the cancer from spreading or shortening your life
Cons:
- It is common to have a raised PSA level, even if you don’t have cancer. This is likely to cause unnecessary stress or anxiety.
- It can miss prostate cancer. 1 in 7 men with prostate cancer would have a normal PSA level.
- If your PSA level is raised, you may need a biopsy to discover what the problem with your prostate is. This can cause side effects such as pain, infection, and bleeding.
A Survivor’s Story: How Screening Saved a Life
One participant, Tony McHale, now 74, joined the study after discovering he carried a BRCA 2 mutation. At 61, his annual PSA screening revealed the early stages of prostate cancer — despite him having no symptoms at all.
“I couldn’t believe it,” McHale recalled. “I felt completely fine. The test and follow-up checks picked up my cancer early. After a three-month course of radiotherapy, I was told I was clear. It felt like I’d been given a new lease of life. Being involved in the study saved my life.”
Contact Us Now To Claim
Compensation for late detection of Prostate Cancer
If you believe your prostate cancer was detected late or that warning signs, PSA results or referrals were missed or delayed, you may be entitled to bring a claim. A delayed diagnosis can have serious consequences for treatment options and outcomes. Find out whether you can take action by visiting our delayed prostate cancer diagnosis claims page for clear guidance on eligibility and next steps.